Intro
This finishes the series of blogs in my RA series that looks to expand upon the article for PhysioFirst which you can read in full here. It has topped 9000 downloads at the time of writing this blog and I am immensely proud of it as a piece of work, it was however hamstrung by a word limit and primarily about the joint dysfunction component of RA. Check out the intro to RA stages here prior to reading this one.
This portion will elaborate on the stage of RA that we are traditionally the most comfortable with, in the literature it has been referred to as the stage after the first two years from diagnosis but this time frame will vary to a degree. People will have very different symptom presentations in this stage and I may have to expand further on this in future blogs.
As usual feedback is gratefully received as are any materials I might be interested in!
PLEASE REMEMBER – THIS BLOG IS NOT A REPLACEMENT FOR CLINICAL REASONING, IF YOU ARE UNSURE GET ADVICE
Established Disease Characteristics
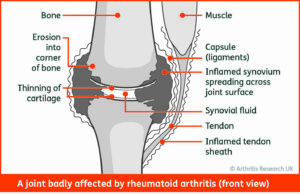
Theoretically we are dealing with a relatively stable disease process at this point which will involve a combination of pain, ongoing inflammation and potentially joint deformity in varying degrees dependent upon the person. In reality there remains the chance of “flares”, acute on chronic periods of inflammation which can signify a lack of control over the condition previously thought to be handled by the current medication regime.
We need to bear in mind when we think about how the person is going to look in this stage that there are likely 5 or more subsets of RA that are as yet undefined. For simplicities sake these might be “erosive”, “non-erosive”, “relapsing-remitting”, “monoarthropathy” and “drug-resistant” (please note I have made these names up to illustrate my point). The number of joints affected, the severity of joint damage (sometimes there will be none) and the regularity of flaring will be affected by multiple factors. Genetics, co-morbidity, time since onset, delay to diagnosis and medication effectiveness (of not more).
Joint deformity is something that will need to be considered in this stage, most likely of the MCPJs and MTPJs but also leading to joint replacements in the usual suspects of the knees, hips and shoulders. It is important to remember that there may be erosive damage without visible joint deformity.
Persistent pain in this cohort is likely under reported in my opinion. These people have had long periods of pain, loss of function, stress and lack of sleep but their pain is often put down to continued disease process whereas there can be no argument against some sensitisation of the nervous system during the period of time when active disease was present.
Symptomatic Treatment
It probably goes without saying after the above section of this blog that this is going to vary significantly from person to person so I have no recipe for you. Umbrella ideas to be considering are education, an exercise program and functional assistance.
Education again is going to vary dependent upon your attendee but don’t assume they have a good handle on the condition, check they know their medicine regimes and that they stick to them! General health advice such as smoking cessation and diet as appropriate. Also consider other co-morbidities especially any that will affect bone or cardiovascular health.
Exercise programs here are again of vital importance, graded exercise programs targeting general strength, cardiovascular fitness, bone density and any functional requirements are key. It may be necessary to be inventive if structural changes prevent specific exercises, lack of wrist extension for example may prevent pushing. With regards to symptom increases there is no evidence that even high intensity exercises are detrimental to symptoms or joints but we need to be pragmatic with increases in the short term. I try to stick to the following advice: pain increases within tolerable levels but not affecting function, swelling/pain/redness is acceptable as long is it reduces back to normal (for the patient) within a few hours and is not worse during the night or first thing in the morning.
Functional assistance can take a few forms, from splints/braces which can be helpful to adaptations of technique or equipment. For example, thickening the handles of cutlery can make it much easier to grip. In all honesty, I often refer to Occupational Therapy colleagues for this portion of management as I have found them exceptionally skilled in this area!
Thanks for reading, I hope you have found this series useful, please sign up to the newsletter here for links to new blogs and extra Rheumatology resources that I find on my travels.
You can now visit my SHOP and find my “Rheumatology At A Glance Booklets“!
Rheumatoid Arthritis Blogs
The Stages of Rheumatoid Arthritis – Early Arthritis
The Stages of Rheumatoid Arthritis – Clinically Suspected Arthralgia
The Stages of Rheumatoid Arthritis
An Introduction to Rheumatoid Arthritis for Therapists
Rheumatoid Arthritis and Pregnancy
References
Brosseau L, Wells G, Tugwell P, Egan, M, Dubulouz C, Casimiro L, Robinson V, Pelland L, Mcgowan J. Ottawa Panel Evidence-Based Clinical Practice Guidelines for Electrotherapy and Thermotherapy Interventions in the Management of Rheumatoid Arthritis in Adults. Physiotherapy 2004:84(11):1016-1043
Brosseau L, Rahman P, Poitras S, Toupin-April K, Paterson G, Smith C, King J, Casimiro L, Angelis G, Loew L, Cavallo S, McEwan J. A Systematic Critical Appraisal of Non-Pharmacological Management of Rheumatoid Arthritis with Appraisal of Guidelines for Research and Evaluation II. PLos ONE 2014 9(5)
Christie A, Dahm k, Moe, R, Haavardsholm E, Hagen K. Effectiveness of Nonpharmacological and Nonsurgical Interventions for Patients With Rheumatoid Arthritis: An Overview of Systematic Reviews. Physical Therapy 2007:87(12):1696-1715
Combe B, Landewe R, Daien C, Hua C, Aletaha D, Alvaro-Gracia J, Bakkers M, Brodin N, Burmester G, Codreanu C, Conway R, Dougados M, Emery P, Ferraccioli G, Fonseca J, Raza K, Silva-Fernandez L, Smolen J, Skingle D, Szekanecz, Kvien T, van der Helm-van Mill A, Vollenhoven R. 2016 Update of the EULAR Recommendations for the Management of Early Arthritis. Annals of the Rheumatic Diseases 2016:0:1-12
Lamb S, Williamson E, Heine P, Adams J, Dosanih S, Dritsaki M, Glover M, Lord J, McConkey, C, Nichols V, Rahman A, Underwood M. Williams M. Exercises to Improve Function of the Rheumatoid Hand (SARAH): A Randomised Controlled Trial and Economic Evaluation. Health Technology Assessment 2015:19(19) ISSN 1366-5278
Lee S, Shin B, Ernst E. Acupuncture for Rheumatoid Arthritis. Rheumatology 2008:47:1747-1753
Loof H, Demmelmaier I, Henriksson E, Lindblad S, Nordgren B, Opava C, Johansson U-B. FearAvoidance Beliefs About Physical Activity in Adults with Rheumatoid Arthritis. Scandinavian Journal of Rheumatology 2015:44:93-99
Markatseli T, Voulgari P, Alamanos Y, Drosos A. Prognostic Factors of Radiological Damage in Rheumatoid Arthritis: A 10-year Retrospective Study. The Journal of Rheumatology 2011:38:44-52
Sharif S, Thomas J, Donley D, Gilleland D, Bonner D, McCrory J, Hornsby W, Zhao H, Lively M, Hornsby J, Always S. Resistance Exercise Reduces Skeletal Muscle Cachexia and Improves Muscle Function in Rheumatoid Arthritis. Case Reports in Medicine 2011:2:205691
Van Den Ende C, Breedveld F, Cessie S, Dijkmans B, de Mug A, Hazes J. Effect of Intensive Exercises on Patients with Active Rheumatoid Arthritis: A Randomised Clinical Trial. Annals of Rheumatological Disease 2000:59:615-621