Intro
This continues the series of blogs in my RA series that looks to expand upon the article for PhysioFirst which you can read in full here. It has topped 9000 downloads at the time of writing this blog and I am immensely proud of it as a piece of work, it was however hamstrung by a word limit and primarily about the joint dysfunction component of RA. Check out the intro to RA stages here prior to reading this one.
This portion will build elaborate on the stage of RA immediately post diagnosis, in the literature this is often referred to as the first 2 years but pragmatically can be thought of the stage after diagnosis but prior to gaining control over the inflammatory process. Our medical colleagues have made strong strides at shortening this phase with work into early recognition, access clinics, aggressive management and new medications enabling better control and improved return to function for many.
As usual feedback is gratefully received as are any materials I might be interested in!
PLEASE REMEMBER – THIS BLOG IS NOT A REPLACEMENT FOR CLINICAL REASONING, IF YOU ARE UNSURE GET ADVICE
Early Disease Characteristics
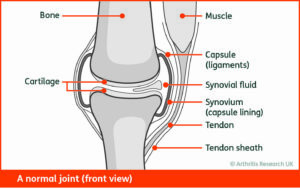
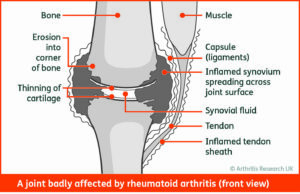
In Early Disease, there are usually no joint erosions or deformities to be contended with, instead acute synovitis causes hot, swollen, stiff and painful joints. This is often coupled with a lack of understanding of the new diagnosis, concern regarding the future and side-effects of new medication. Patients often find hand functions extremely restricted as the MCPJs have decreased range of motion and increased pain with gripping activities, this is particularly exaggerated in the morning. Similar problems befall the feet as the Metatarsal-Phalangeal Joints (MTPJs) are often affected, the same swelling, temperature, stiffness and pain are present affecting any weight bearing activities and driving.
It is important to keep up to date with the progress of the patient with their medical management during this stage. Medicine changes, escalation and titration are often frequent as the Rheumatologists try to gain as much control as possible as quickly as possible, this is often hampered by weaning of oral steroids or side-effects from the medications. An understanding of the time it takes many of these drugs to take an effect upon symptomology is important (and outside the scope of this blog).
Some patients will gain symptomatic control but retain some “subclinical synovitis” while not necessarily the majority of us clinicians will need to worry about it is something to consider if you can perform Diagnostic Ultrasound, this is an area Rheumatologists are exploring further.
Symptomatic Treatment
Treatment in this stage of RA falls in to two broad sections, Education and Maintaining Function. Unfortunately, Physios are not that useful in the early stage at actually managing synovitis caused by an auto-immune condition however there are a lot of things that we can do to help the individuals.
Education at this stage is of the disease process is of vital importance, topics covering the pathophysiology of the condition, signposting to NRAS, maintaining activity levels and assisting with modifying these as necessary should be covered as quickly and with as much detail as possible tailoring the advice to the individual. The more function that can be retained the better the outcomes will be later. There are studies that show there is no long-term ill effects to maintaining exercise levels even at high intensity in this population and this can be reassuring to patients. In my experience meeting somewhere in the middle at this point is sensible, although no harm will come to patients with intense exercise with florid synovitis, it certainly isn’t nice and not everyone is up for it! Practically I will say something along the lines of “you are ok to run/lift weights etc” but then open it up to the patient to actually make the suggestions and decisions on the amount/intensity of the activity. Through the process maintain a reassuring and encouraging narrative that they can try higher intensity activities alongside their chosen ones.
Adding in specific exercises at this stage is entirely dependent upon the individual, maintaining range of motion I think should be a priority especially in the hands, any strength exercises on top of this are a bonus and CV work another bonus. Aim for maintenance but increase to tolerance!
Reassure and provide ways tailored to the individual to help them to continue functioning at as higher level as possible. Retaining work status is vital to outcomes so pacing, adapting activities and where appropriate liaising with employers may be necessary in the short to medium term.
Beginning a Hand exercise program such as the one included in the SARAH trial is recommended regardless of the symptoms presenting in the hands. Specific hand therapy is a good option if available, splinting both functional and resting is required to be bespoke and dealt with by those with experience.
Adjunct therapies are likely to be of minimal benefit and I would not advocate the use of acupuncture/dry needling for those on immunosuppressive medications and/or systemic inflammation.
Future Proofing
As mentioned above, starting reassurance and education early is important. Advise why there is a need to improve general health practices, maintain and in all likelihood increase exercise levels. Smoking cessation is necessary due to its deleterious effects on disease outcomes and medication effectiveness. Sleep, dietary intake and stress management strategies are all lines of education to explore with each individual.
Ensure they are aware of all the stakeholders in their care and the role they play (this will vary dependent on location and pathways) and how they can access these stakeholders when required.
Thanks for reading, there is one more stage left for me to write about so if you would like to be kept updated then sign up to the newsletter here for links to new blogs and extra Rheumatology resources that I find on my travels.
Rheumatoid Arthritis Blogs
The Stages of Rheumatoid Arthritis – Clinically Suspected Arthralgia
The Stages of Rheumatoid Arthritis
An Introduction to Rheumatoid Arthritis for Therapists
Rheumatoid Arthritis and Pregnancy
References
Brosseau L, Wells G, Tugwell P, Egan, M, Dubulouz C, Casimiro L, Robinson V, Pelland L, Mcgowan J. Ottawa Panel Evidence-Based Clinical Practice Guidelines for Electrotherapy and Thermotherapy Interventions in the Management of Rheumatoid Arthritis in Adults. Physiotherapy 2004:84(11):1016-1043
Brosseau L, Rahman P, Poitras S, Toupin-April K, Paterson G, Smith C, King J, Casimiro L, Angelis G, Loew L, Cavallo S, McEwan J. A Systematic Critical Appraisal of Non-Pharmacological Management of Rheumatoid Arthritis with Appraisal of Guidelines for Research and Evaluation II. PLos ONE 2014 9(5)
Christie A, Dahm k, Moe, R, Haavardsholm E, Hagen K. Effectiveness of Nonpharmacological and Nonsurgical Interventions for Patients With Rheumatoid Arthritis: An Overview of Systematic Reviews. Physical Therapy 2007:87(12):1696-1715
Combe B, Landewe R, Daien C, Hua C, Aletaha D, Alvaro-Gracia J, Bakkers M, Brodin N, Burmester G, Codreanu C, Conway R, Dougados M, Emery P, Ferraccioli G, Fonseca J, Raza K, Silva-Fernandez L, Smolen J, Skingle D, Szekanecz, Kvien T, van der Helm-van Mill A, Vollenhoven R. 2016 Update of the EULAR Recommendations for the Management of Early Arthritis. Annals of the Rheumatic Diseases 2016:0:1-12
Lamb S, Williamson E, Heine P, Adams J, Dosanih S, Dritsaki M, Glover M, Lord J, McConkey, C, Nichols V, Rahman A, Underwood M. Williams M. Exercises to Improve Function of the Rheumatoid Hand (SARAH): A Randomised Controlled Trial and Economic Evaluation. Health Technology Assessment 2015:19(19) ISSN 1366-5278
Lee S, Shin B, Ernst E. Acupuncture for Rheumatoid Arthritis. Rheumatology 2008:47:1747-1753
Loof H, Demmelmaier I, Henriksson E, Lindblad S, Nordgren B, Opava C, Johansson U-B. FearAvoidance Beliefs About Physical Activity in Adults with Rheumatoid Arthritis. Scandinavian Journal of Rheumatology 2015:44:93-99
Markatseli T, Voulgari P, Alamanos Y, Drosos A. Prognostic Factors of Radiological Damage in Rheumatoid Arthritis: A 10-year Retrospective Study. The Journal of Rheumatology 2011:38:44-52
Sharif S, Thomas J, Donley D, Gilleland D, Bonner D, McCrory J, Hornsby W, Zhao H, Lively M, Hornsby J, Always S. Resistance Exercise Reduces Skeletal Muscle Cachexia and Improves Muscle Function in Rheumatoid Arthritis. Case Reports in Medicine 2011:2:205691
Van Den Ende C, Breedveld F, Cessie S, Dijkmans B, de Mug A, Hazes J. Effect of Intensive Exercises on Patients with Active Rheumatoid Arthritis: A Randomised Clinical Trial. Annals of Rheumatological Disease 2000:59:615-621


