Intro
This is the third blog of my RA series that looks to expand upon the article for PhysioFirst which you can read in full here. It has topped 9000 downloads at the time of writing this blog and I am immensely proud of it as a piece of work, it was however hamstrung by a word limit and primarily about the joint dysfunction component of RA. Check out the intro to RA stages here prior to reading this one.
This portion will build elaborate on the first stage of RA which is the pre-diagnosis stage, it is worth remembering that guidelines state Rheumatoid Arthritis must be diagnosed by a Rheumatologist. This means regardless of the presenting symptoms or stage at which the patient presents to you in clinic if they haven’t been diagnosed by a Rheumatologist they technically don’t have RA yet.
As usual feedback is gratefully received as are any materials I might be interested in!
PLEASE REMEMBER – THIS BLOG IS NOT A REPLACEMENT FOR CLINICAL REASONING, IF YOU ARE UNSURE GET ADVICE
Clinically Suspect Arthralgia
Imagine for a minute if you will that a patient arrives in your clinic, their story unfolds as one containing a history of symptoms such as MCPJ swelling, pain and early morning joint stiffness lasting for over 60 minutes, further questioning reveals the patients sister has RA. This is a strong indicator that we should include Rheumatoid Arthritis in our differential diagnosis, at this stage we will place this patient into the category of “Clinically Suspect Arthralgia” (CSA) i.e. Joint symptoms we think could develop into RA.
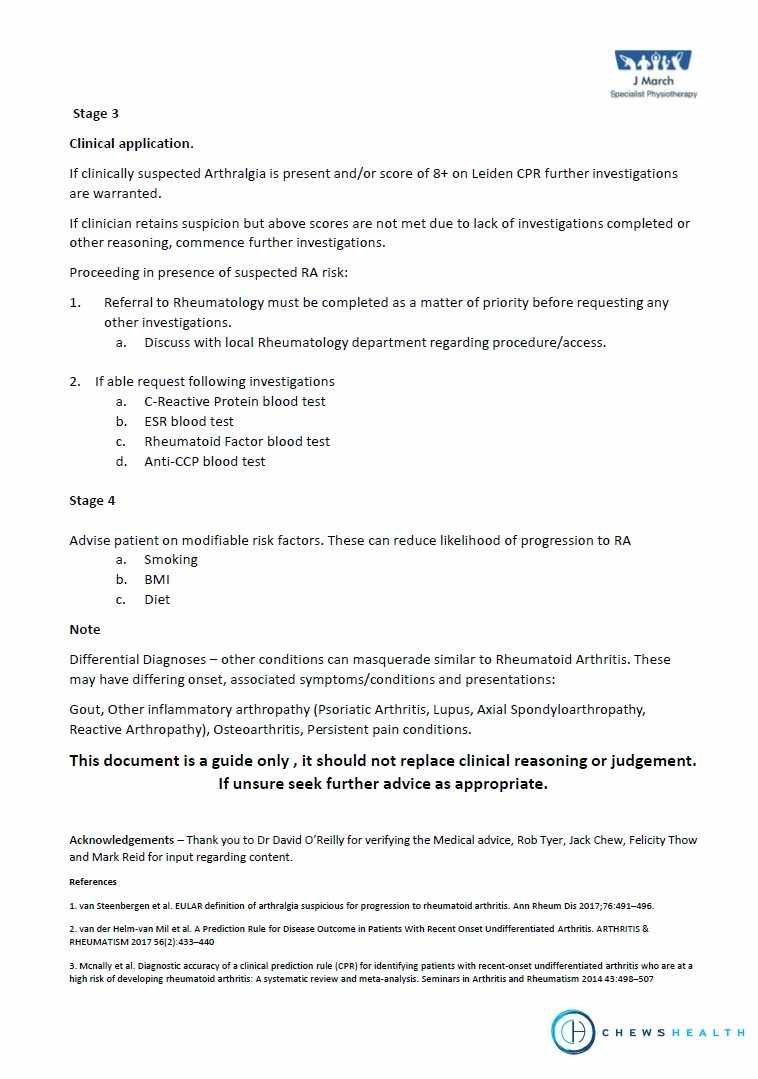
My advice is at this stage to be prepping the patient for a referral to Rheumatology, explaining why you are recommending the referral and the process this will take. It is of paramount importance that this happens as quickly as the pathway allows as delay to diagnosis has a direct effect on outcome. The logistics of the referral will depend upon your local pathways and your position within them. It is worth knowing these or having somewhere easy to reference for when the time comes, awareness of the appropriate locations and clinics available to refer to will speed up the process.
Assessment
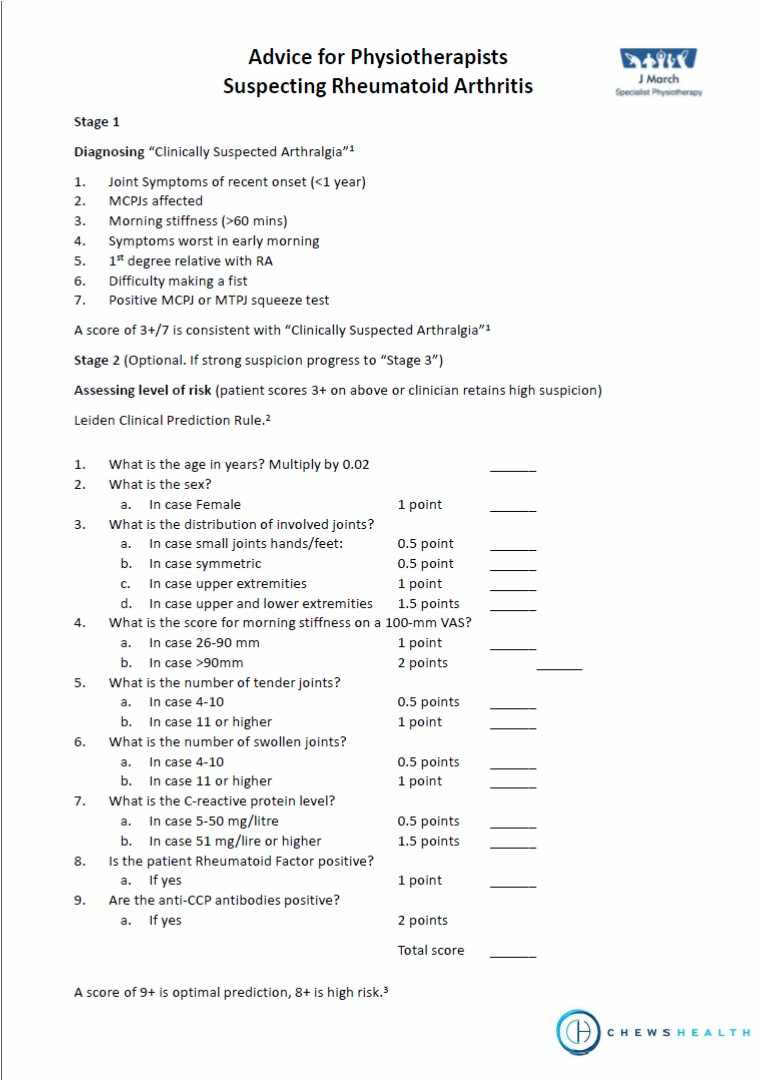
If your clinical reasoning senses are tingling I have you covered for a bit more detail and the questions to ask. Check out page 1 of my “Suspecting RA” document for scoring systems to assess the risk likelihood of CSA. The first score relates to CSA specifically, the second is the Leiden scale which gives a risk score of developing Rheumatoid Arthritis more specifically but requires further information such as blood results. Neither are perfect and by no means are definitive but they make a very nice guidance and add some weight to referral letters.
Referral
As mentioned above this is going to depend greatly on your local referral pathways and your position within them. Ideally refer directly to an appropriate Rheumatology, early access clinic. Include in your referral letters specifics such as duration of early morning joint stiffness, family history, the joints affected and any investigations already undertaken so that it is clear what you are referring for.
Investigations
Where appropriate and within your scope of practice refer for investigations, bloods including FBC, ESR, CRP, RF and Anti-CCP* are necessary (*check locally regarding requesting this test as some locations don’t allow request outside of secondary care). Ultrasound scan is the imaging of choice to look for Synovitis. For more detail on bloods check out my previous blog here.
Please note – even if you request bloods, refer to Rheumatology and allow the Rheumatologist to make the clinical judgement on their relevance.
Advice
The benefit of catching patients early in their RA journey is that it is possible to induce remission in some cases. A lot of this is down to early and aggressive medical management but there are some things that the patients can do to increase the likelihood of this. It is well within a Physios remit to give the following advice.
Stop smoking. If we needed more reasons to discuss smoking cessation this yet another to add to the very long list. Even a modest reduction (ideally completely stopping) not only increases the likelihood of remission but also reduces the severity of inflammatory disease and increases the effectiveness of medications.
Reduce BMI. Fat cells, especially abdominal ones, are immunologically active releasing inflammatory cytokines into the system. This will exacerbate any symptoms of RA and make it harder to control.
Improve Diet. While no specific advice exists here, a Mediterranean style diet is the usual go to. Reduction of processed foods and alcohol will help with general health as well as assist with reducing the aforementioned BMI.
Reassurance
As physios we need to promote robustness and reassure that physical activity/exercise remains of vital importance. There is no evidence that even high intensity exercise has a deleterious effect on outcome but the benefits are numerous. Encourage patients to stay active, keep up their hobbies and stay in work as far as is reasonable and the outcomes are almost universally improved.
Thanks for reading, the stages of the condition will be expanded upon soon so if you would like to be kept updated then sign up to the newsletter here for links to new blogs and extra Rheumatology resources that I find on my travels.
Rheumatoid Arthritis Blogs
The Stages of Rheumatoid Arthritis
An Introduction to Rheumatoid Arthritis for Therapists
Rheumatoid Arthritis and Pregnancy
References
van Steenbergen HW, Aletaha D, Beaart-van de Voorde LJJ, et al. EULAR definition of arthralgia suspicious for progression to rheumatoid arthritis Ann Rheum Dis 2017;76:491–496.
van der Helm-van Mil et al. A Prediction Rule for Disease Outcome in Patients With Recent-Onset Undifferentiated Arthritis ARTHRITIS & RHEUMATISM Vol. 56, No. 2, February 2007, pp 433–440.
McNally et al. Diagnostic accuracy of a clinical prediction rule (CPR) for identifying patients with recent-onset undifferentiated arthritis who are at a high risk of developing rheumatoid arthritis: A systematic review and meta-analysis Seminars in Arthritis and Rheumatism 43(2014)498–507.
van Beers-Tas MH, et al., How does established rheumatoid arthritis develop, and are there possibilities for prevention?, Best Practice & Research Clinical Rheumatology (2015),