As we move forwards in medicine with the understanding of Spondyloarthritis, some things are becoming more complex and others more simple. (I say we, I have nothing to do with it, it’s the amazing researchers and Rheumatologists that deserve all credit). In other news there is now a Rheumatology.Physio Facebook page! Go follow there for updates and news!
Please consider heading to the shop to find more resources, I have got a few Spondyloarthritis related ones and an overview doc HERE and supporting me to continue this hairbrained project! You can also listen to all of my blogs as podcasts subscribe to your preferred channel HERE
please do consider going to the shop to grab yourself some resources. It supports me to keep creating resources, plus I genuinely believe them to be helpful to practice!
As usual feedback is greatly appreciated and any further reading for me please send it my way!
PLEASE REMEMBER – THIS BLOG IS NOT A REPLACEMENT FOR CLINICAL REASONING, IF YOU ARE UNSURE GET ADVICE
Introduction
Spondyloarthritis is an umbrella term covering a number of clinical diagnoses that can be broadly described as “enthesitic” in nature. This is an oversimplification but I find it helpful to understand where the site of inflammatory effect is and why certain extra articular features manifest. (MORE HERE).
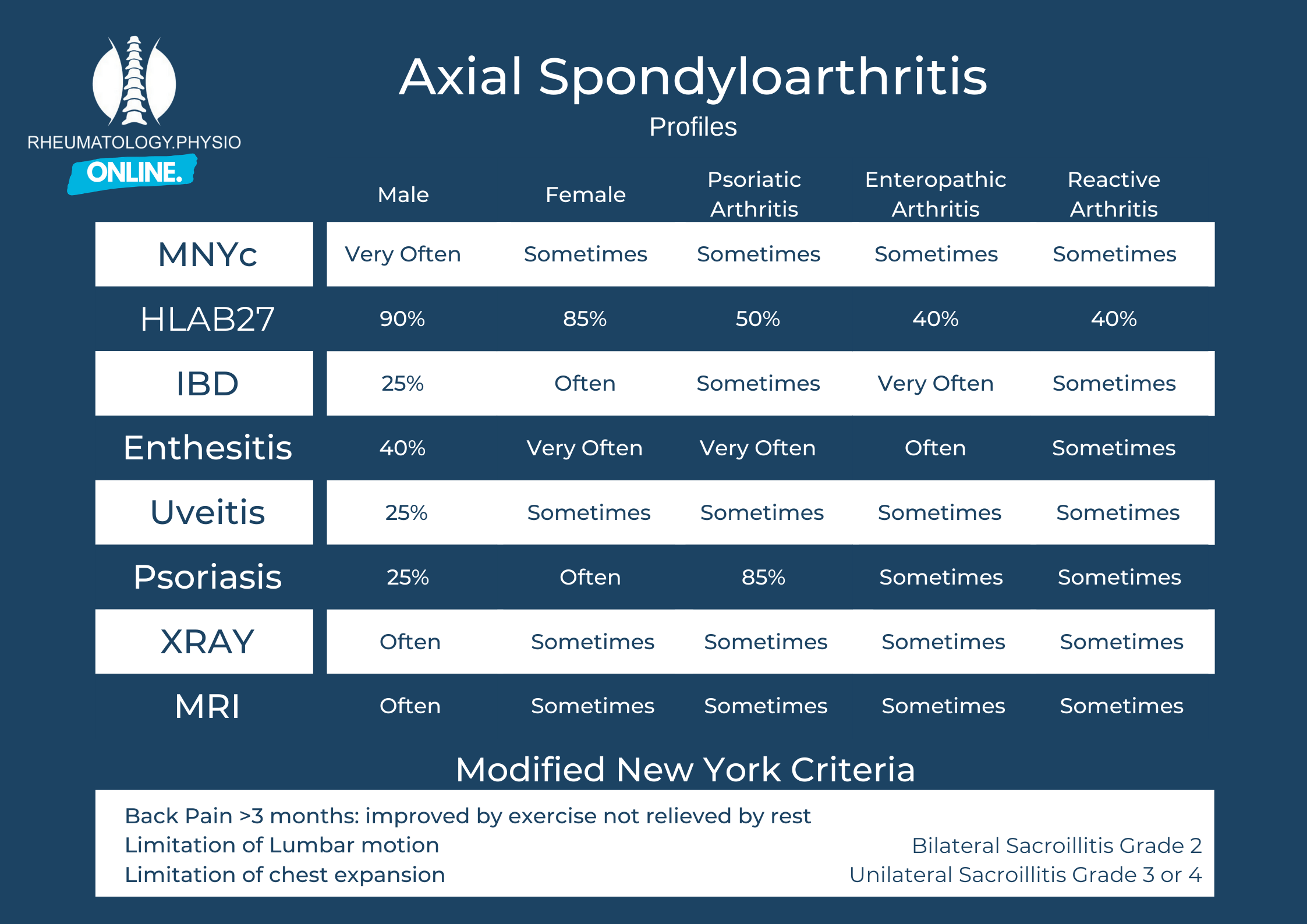
Once determined as a Spondyloarthritis we can break these down into different terms based on clinical and radiological features. This is useful for Rheumatologists and researchers because these different presentations respond differently to both time and medications. They are also more or less prevalent with demographic variables.
While as Therapists we are unlikely to need to make these distinctions ourselves it is important to know about them to aid with our clinical reasoning in recognition roles, education and when receiving referrals.
Axial vs Peripheral Spondyloarthritis
This refers to the predominance of clinical symptoms. Axial Spondyloarthritis (AxSpA) will have predominantly spinal and sacroiliac joint symptoms (but may also have peripheral manifestations) and Peripheral Spondyloarthritis (PSpA) will have predominantly peripheral symptoms (but may also have axial manifestations).
Of note, this may change throughout the course of the disease but it is probably unnecessary to keep changing the diagnosis.
R-AxSpA vs Nr-AxSpA
This one is a simpler difference and is based on radiological findings and a clinical diagnosis of AxSpA.
Radiographical Axial Spondyloarthritis (R-AxSpA) shows changes on Xray sufficient to meet specific criteria, None Radiographical Axial Spondyloarthritis (Nr-AxSpA) doesn’t show these changes. It does not depend on inflammatory changes on MRI.
A proportion of Nr-AxSpA diagnoses will develop into R-AxSpA (Younger, HLA-B27+ve, Males are most likely).
It is extremely important to note that the disease burden of both classifications are EQUAL.
R-AxSpA vs Ankylosing Spondylitis
“Almost all patients with axSpA with radiographic sacroiliitis fulfil both ASAS and mNY criteria , which supports the interchangeable use of the terms AS and r-axSpA” – https://ard.bmj.com/content/78/11/1545
Enteropathic Spondyloarthritis
Occurring in those with Inflammatory Bowel Disease this can be any of the combinations mentioned above subsequent to a diagnosis of conditions such as Crohns disease and Ulcerative Colitis.
Symptom Profiles
This certainly isnt perfect but it gives you a good idea of the different presentation profiles, there is a lot of overlap!
End
I hope you find this blog useful separating out the various terms you may hear. I don’t think as referring clinicians we need to be this specific and clearly we cant be in some cases where xrays etc haven’t been performed.
Get me any feedback you might have so that I can grow and improve.
See you next time!
Boel A, Molto A, van der Heijde D, et alDo patients with axial spondyloarthritis with radiographic sacroiliitis fulfil both the modified New York criteria and the ASAS axial spondyloarthritis criteria? Results from eight cohortsAnnals of the Rheumatic Diseases 2019;78:1545-1549.


