Starting with some Thanks for this blog. Thank you to Professor Bhaskar Dasgupta who ran a brilliant webinar (25/11/2020) on Polymyalgia Rheumatica (PMR). Find more out about him here. There was so much contained in 45 minutes and I have tried to condense it down to the applicable information for us MSK therapists.
Here is my previous blog on PMR from over 2 years ago!
As usual feedback is greatly appreciated and any further reading for me please send it my way!
PLEASE REMEMBER – THIS BLOG IS NOT A REPLACEMENT FOR CLINICAL REASONING, IF YOU ARE UNSURE GET ADVICE
Blog Available as a Podcast here
Introduction
Polymyalgia Rheumatica is a systemic inflammatory condition affecting older people (>50), it overlaps with a number of conditions but is actually most closely linked to vasculitis. It can present with some peripheral synovitis but is primarily a proximal condition affecting the shoulders and pelvic girdle/hips.
As far as I can work out at this current time, Rheumatologists and Researchers are still unsure as to the exact pathophysiology of PMR and as such it is to a degree, a diagnosis of exclusion.
Treatment is primarily with steroids and occasionally DMARDs when there is peripheral synovitis. There is no guidance around management from a rehab/physio perspective and my advice is to manage these as able from an individual functional perspective.
Features
PMR usually presents as an acute onset of inflammatory pattern pain and stiffness of both shoulders and/or both hips in people age 50+ (Peak onset is 65). These symptoms cover a significant area of the shoulders and hips/pelvic area.
Approximately 739 cases per 10000 people, 3 times more common in females than males. While it is common it is also often misdiagnosed and has an average delay to diagnosis of 13 months from onset.
Approximately 1/3 of patients will go on to develop Rheumatoid Arthritis and 23% will have perpheral synovitis. It is very unusual to not have a raised CRP and/or ESR on blood testing.
Positive Features (not diagnostic but make PMR more likely)
- Acute onset (new) bilat. Shoulder and or Buttock pain
- Early morning stiffness lasting 45+ mins
- Night pain with severe stiffness
- Fever, weightloss, fatigue
- Age 50+
- Raised ESR and/or CRP
Negative Features (don’t rule out PMR but make it less likely)
- Positive anti-ccp or RF or ANA etc (other clinical diseases more likely)
- Presence of peripheral arthritis
- Presence of headache, jaw claudication, visual symptoms (GCA)
Imaging
While I would recommend basing your differential diagnosis off clinical symptoms at this current time, if imaging has already been done or you have point of care ultrasound available then this may be of benefit.
PMR patients often show bilateral subdeltoid bursitis and/or bilateral biceps tendinosis and/or bilateral hip bursitis.
Differential Diagnosis
Consider other meaningful clinical conditions which may present with bilateral shoulder and/or bilateral hip pain. Including but not limited to:
Fibromyalgia, Osteoarthritis, late onset AxSpA, sinister pathology.
Ensure you discuss, headaches, jaw claudication and vision. These raise the possibility of Giant Cell Arteritis (PMR symptoms would be a potential feature of this condition)
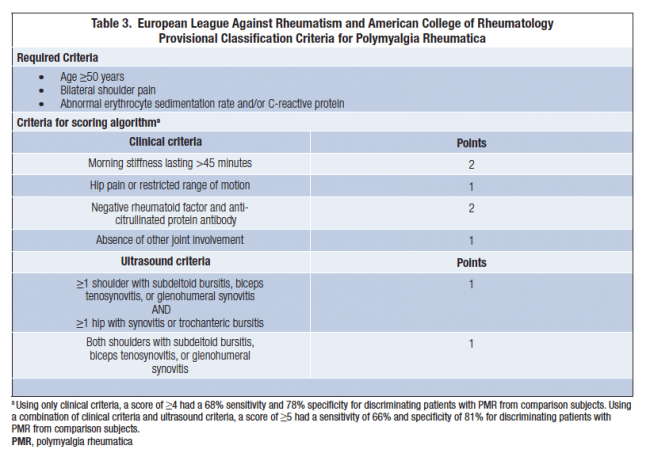
Use the below PMR Probability score to help you with your reasoning.
Onward referral
Refer suspected PMR patients to Rheumatology for definitive diagnosis and commencement of management. Make sure to check your local pathways as these may vary.
End
I hope that this helps you with your recognition of Polymyalgia Rheumatica. Please do consider heading to my shop to support me to continue creating these resources!
Get me any feedback you might have so that I can grow and improve.
See you next time!


