I think this is the most common question I have been asked over the last few years since I started to be more vocal about Rheumatology Conditions. I used to answer it as best I could but always ended up rambling off in different directions. In this blog I will endeavour to explain why and hopefully suggest we put this specific question to bed.
The new recurring features are back too “Legend of the Blog” and if you scroll all the way to the bottom you can listen to the music I was listening to when I wrote this.
Please consider heading to the shop to find more resources and supporting me to continue this hairbrained project!
As usual feedback is greatly appreciated and any further reading for me please send it my way!
PLEASE REMEMBER – THIS BLOG IS NOT A REPLACEMENT FOR CLINICAL REASONING, IF YOU ARE UNSURE GET ADVICE
Legend of the Blog
This weeks legend is Erik Meira whose podcast (with JW Matheson) really kicked off my inquiry and critical thinking about research and its relationship to practice. It also really helped me formulate plans and ideas around a lot of the materials I have created since. Follow his twitter page, check out his website and listen to the podcast especially if you like puns and Less Than Jake…
Introduction
Ok let’s set this up properly. Osteoarthritis vs Rheumatoid Arthritis is not some sort of match or comparison but really it’s a question aimed at elaborating on assumed different pathophysiology’s and symptom presentations. It makes superficial sense, OA is the most common form of arthritis and RA is the most well known overtly inflammatory arthritis (although Gout is more prevalent and OA is arguably inflammatory… we will come back to this). Differentiating between the two is very important, delay to diagnosis in RA leads to poorer outcomes, OA being so highly prevalent means you will find it very regularly in RA patients and so misdiagnosis is easy.
It is also very easy to become slightly blinkered in practice, OA is very prevalent and RA is comparatively rare, I think in some ways its an awareness of this that makes MSK clinicians keen to rule out RA in the presence of OA.
There are a few issues here that mean I sometimes digress off into tangents when trying to differentiate the two conditions and these are:
- Osteoarthritis has a significant inflammatory component
- There are other clinically relevant conditions that overlap these two
- The lines are sometimes blurry enough that we can’t differentiate without specialist opinion
- Imaging and Bloods need to be specific for the conditions you are looking at
OAvsRa…
So there are in general some differences between OA and RA and I have listed them here:
- Onset in RA is usually younger (30-60 peak vs 50+ for OA)
- RA typically involves multiple joints, OA typically 1 or 2
- RA typically involves the small joints of the hands and feet, OA Hip, knee or 1st CMC (thumb)
- RA typically presents with an inflammatory pattern (protracted early morning symptoms >30 mins)
- RA is associated with a family history of RA
- RA patients are commonly (95%) anti-ccp positive.
This remains problematic because there are a number of outliers in both conditions, early onset OA, late onset RA for example. Variable joint patterns in both conditions is reasonably common, joint symptoms with RA may not reach 30 mins and OA may surpass 30 mins… I could go on.
We need to take the whole picture and make a clinical decision, that decision may be “I don’t know” and that’s ok. There is help at hand with my Recognising RA guide here
Pathophysiological issues
Well, why is this so difficult then I hear people ask. Why can’t we easily differentiate possibly the most common MSK condition in the world from a relatively rare one?
Well, the challenge comes in a couple of forms, as mentioned above the symptom profiles overlap significantly especially when you get into fringe cases which in OA is not that rare because there are so many of them. Not to mention because of OAs prevalence, many RA patients also have OA.
Imaging and blood testing are just as challenging ground with false negatives and positives in both conditions or Anti-CCP being unavailable in primary care in many locations.
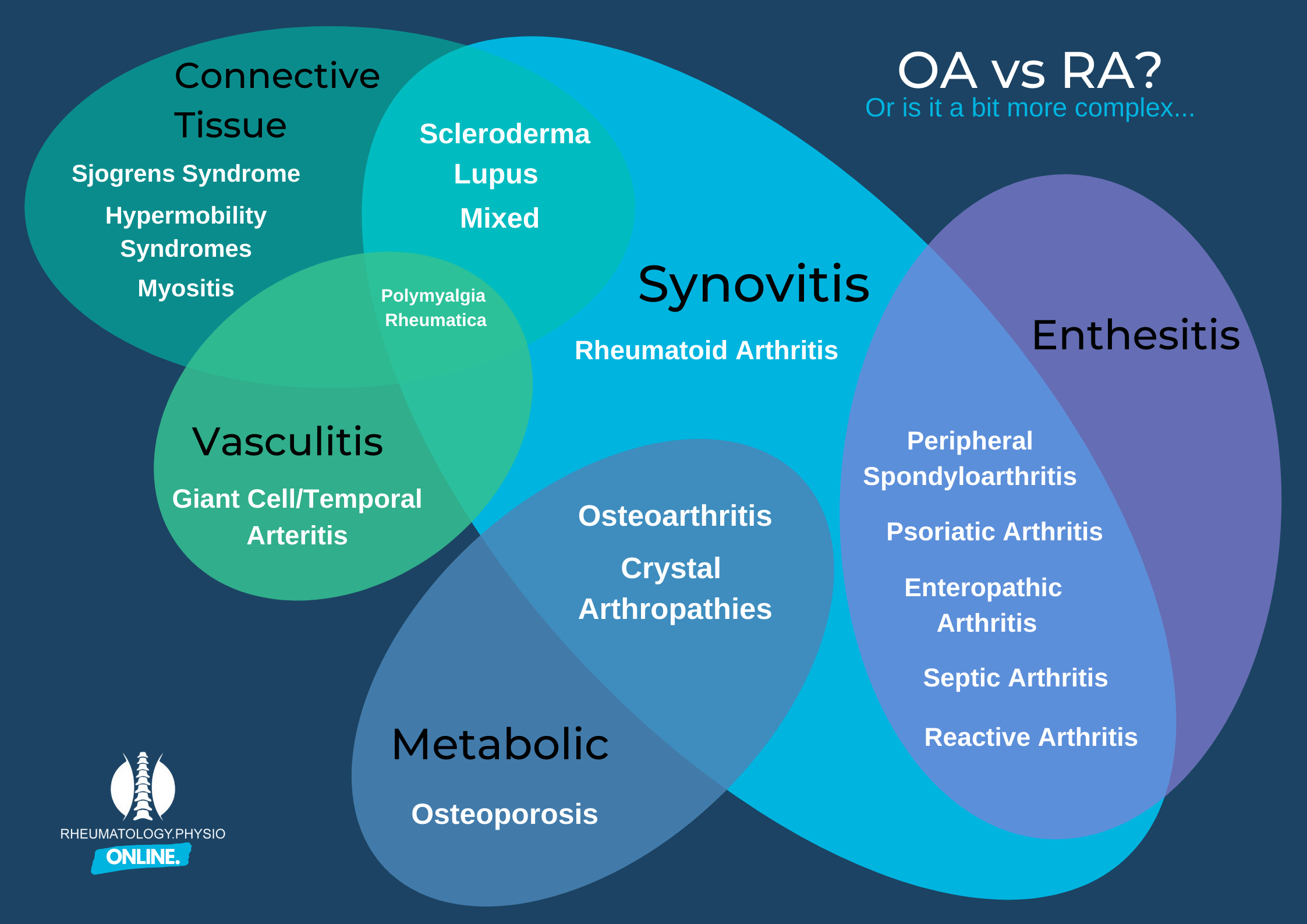
There are also other clinically important conditions that overlap as well. Too many times have I seen a clinician appropriately rule out RA and not recognise gout, Psoriatic Arthritis, lupus and so on. This is where we must be well rounded in our understanding of various masqueraders. You can see from the image below some of this complexity.
Finally a misunderstanding of Osteoarthritis is a contributing factor. Our understanding has moved on to categorising it as a metabolic disorder or a low grade inflammatory arthritis rather than one of predominantly mechanical stress. Once you consider this it becomes more obvious why it overlaps with the other inflammatory disorders so much.
End
I hope you have enjoyed this blog and that we make sure we understand the symptom profiles, presentations and investigations to ensure we manage the people who attend our clinics appropriately. You can find plenty more information on these inflammatory disorders across my blog pages. My final advice is to remember that OA is extremely common and RA relatively rare, clinically reason appropriately to rule out none OA causes and you will be right far more often than you are wrong.
Get me any feedback you might have so that I can grow and improve.
See you next time!
Music Choice: Billy Talent – “Devil on My Shoulder”
“As I get closer, my dreams get farther
I climb the ladder, but you kick it over
Thirsty for water, you give me vinegar
When I drink your medicine, it just makes me sicker… “


